The Brain + Body Health Connection
Many people think of physical and mental health as separate entities. However, with the help of continually advancing technology, researchers and medical professionals have learned that the brain and body are more connected than we once thought. With brain imaging, we can now see that the brains of people with depression have physical differences compared to the brains of individuals who do not have depression.
Luckily, we have also learned that our brains have an incredible ability to repair themselves when given the right tools. One of the physical differences we often see in a depressed brain compared to a non-depressed brain is that portions of the brain have atrophied. When treated with the right tools, we can see these atrophied parts of the brain begin to regrow. This regrowth typically results in a lift in depressive symptoms for many patients.
At Manlove Brain and Body Health, we work with our patients to develop a personalized psychiatric treatment plan that often incorporates whole-body health. This is because the things that give our body what it needs to function at its best—vitamins, minerals, exercise, rest—are also needed to help keep our brain healthy. When our patients make healthy lifestyle changes in combination with psychiatric interventions, we see our patients respond better and faster to their mental health treatments.
Below is a summary of the What’s Killing Us in 2023 talk given by cardiologist Jose Teixeira, MD as part of our Brain + Body Health Talks series. Dr. Teixeira’s talk outlines specific steps that you can take to improve your heart health. When we focus on improving our heart health, we are also giving our bodies the tools they need to manage and prevent mental illnesses.
What’s killing us in 2024
What’s killing us in 2024 is not what you may think. Most people think that sudden cardiac death is rare, but it’s not. It’s the number one cause of death in the U.S.
In medicine, we’re very good at putting out the fires. We can be very successful at treating heart attacks, strokes, and cardiovascular disease, but we are failing miserably in prevention, which would stop these fires from starting.
Sudden cardiac death (SCD) is a death caused by a heart problem that occurs within one hour of the onset of symptoms. You’re fine and then in one hour, you’re gone. This makes up 50% of all cardiac deaths. This is different from a heart attack, which is caused by a blockage in one of the arteries of the heart. Sudden cardiac death is an electrical problem, while a heart attack is a plumbing issue.
80% of out of hospital cardiac arrests occur at home.
40% are unwitnessed.
Causes of Death in the U.S.
- 2021
- 700,000 heart disease
- 605,000 cancers
- 415,000 COVID-19
- 188,000 COVID-19
- 2022
- 699,000 heart disease
- 607,000 cancers
- 218,000 unintentional injuries
- 188,000 COVID-19
Who is affected?
Sudden cardiac death affects 1,000 Americans per day. People who already survived one episode of cardiac arrest are at high risk due to the underlying damage to their heart muscle. However, most people who die from cardiac arrest are not considered high risk. They have some heart condition, but they are not candidates for any specific intervention or defibrillator.
Cardiologists spend our lives taking care of the high risk people, but we’re missing the majority. The most effective treatment we have today to prevent sudden cardiac death is implanting a defibrillator, a sort of a pacemaker that constantly detects what the heart is doing and will deliver a small shock if it detects racing. While we place more than 100,000 defibrillators per year in the U.S., this is not an option for most people who die from sudden cardiac death.
The underlying cause of sudden cardiac death
Coronary artery disease, which is a blockage in the arteries of the heart, is the underlying cause of 80% of SCD cases. If we could get rid of the blockage in the arteries of the heart, sudden cardiac death would not be an issue.
In 2000, Erika Frank, MD published a study in the American Journal of Preventive Medicine on mortality rates and causes among U.S. physicians (AJPM). She looked at the mean age of death for people who died between 1984 and 1995 in white and black men.
Mean Age at Time of Death
- White Men
- General population
- Professionals
- White Men
- 70.3 years
- 70.9 years (lawyers 72.3 years, doctors 73 years)
- Black Men
- 63 years
- 65 years (doctors 68 years)
The bottom line is physicians’ top 10 causes of death were the same as that of the general population. Among doctors, our mean age of death is slightly higher, but not by much. While we may know better, we live similar lifestyles as everyone else. We work hard, we’re stressed out, we eat junk just like everybody else, so we die just like everybody else.
However, looking at the rates among black men, we see that knowledge is power. Black male physicians lived an average of 5 years longer than the general population.
Warning Signs
There may be some warning signs of cardiac arrest, but they’re not very good.
- Chest pain – you may experience chest pain in the left side of the chest, left shoulder, jaw, neck, or down the arms, the same as a heart attack
- Shortness of breath
- Fainting
- Palpitations – pounding in the chest
- Sweating – profuse sweating for no apparent reason
- No symptoms (most common)
In most cases, there are no warning signs. Sudden cardiac death is the first and last symptom.
Risk Factors of Sudden Cardiac Death
Risk factors of sudden cardiac death include:
- Alcohol consumption. Consuming more than 5 drinks a day causes damage to heart, liver, and pancreas. It is recommended that men have no more than two drinks a day and women have no more than one drink a day.
- Smoking. Smoking increases risk of lung cancer, oral cancer, bladder cancer, destroys lungs causing chronic obstructive pulmonary disease (COPD), and sudden cardiac death. The rate of smoking in the U.S. has dropped dramatically, but 20-25% of Americans still smoke.
- Stress.
- Cocaine. Cocaine can cause sudden cardiac death in young people.
- Dialysis. 25% of people on dialysis die suddenly. Dialysis is not a perfect replacement for your kidneys. There is a 3-fold increase in SCD 12 hours prior to the next dialysis session.
- Exercise. There is a little bit of risk associated with exercise, especially in people with cardiac disease. However, the benefits of exercise clearly outweigh the risks, even for those with cardiac disease. In fact, the best place to have a cardiac arrest is at a cardiac rehab center, and the next best place is in a gym. There will be witnesses and nearly all gyms now have a defibrillator with staff trained to use them.
Prevention Through Lifestyle Medicine
If most of the people who are going to have a cardiac arrest are not at a higher risk and can’t have a defibrillator put in, can we prevent it in other ways? Yes! Lifestyle changes can significantly lower your risk of sudden cardiac death.
Improve overall health
Don’t look for a miracle food or medication, look at your overall health. Consider how you can improve your diet, activity level, and stress level.
In the Nurses’ Health Study which followed 121,000 nurses, it was found that a low risk lifestyle led to an 81% reduction in SCD (NCBI). A low-risk lifestyle consisted of 4 factors:
- No smoking
- BMI 21-24.9
- Exercising 30 min/day
- Alternate Mediterranean diet
- High intake of fruits, vegetables, nuts, legumes, fish, whole grains
- Moderate intake of alcohol, low intake of red and processed meat
Shockingly, only 3% of nurses met all 4 of these criteria.
The best way to improve your overall health is to start with small lifestyle modifications. Here are a few options to consider starting with.
Eat Well – Go Nuts
Eat four servings of nuts per week.
Consuming nuts decreases your risk of sudden cardiac death. In a study of 21,454 physicians who were observed over a period of 17 years, the Harvard School of Public Health found that consuming two or more servings of nuts per week reduced sudden cardiac death by 48% and coronary heart disease death by 30% (JAMA Internal Medicine).
In the Adventist Health Study which followed 34,192 Seventh-day Adventists, those who consumed 5 or more servings of nuts per week decreased sudden cardiac death by 48% and nonfatal heart attacks by 51%.
Any kind of nuts are a great source of protein, antioxidants, and fiber. Nuts lower high blood pressure, lower bad cholesterol, increase good cholesterol, reduce inflammation, improve artery health, decrease the risk of blood clots (which cause heart attacks and strokes), and lower the risk of sudden cardiac death.
Brazil nuts are great for you. A study gave one serving (4 Brazil nuts) to a bunch of young people and measured their cholesterol levels at various times. 9 hours after eating the Brazil nuts, their bad cholesterol decreased and good cholesterol increased. After 30 days, good cholesterol remained elevated and bad cholesterol stayed down.
My 5 rules when buying nuts (2 R’s, 3 U’s):
- Buy Raw
- Dry Roasted
- Unsalted
- Unsweetened
- Unpeeled – 50% of antioxidants are in the thin layer encasing the nut (not the shell)
If you’re trying to lose weight, don’t overdo it because they have a lot of fat in them. They are good fats though and many people who start eating nuts tend to lose weight.
Spice it up! The hotter the better.
Spice your food with chili peppers. Chili peppers have many health benefits. The hotter the pepper, the more health benefits it has. If you don’t have an appetite for spicy food, sweet peppers still have a lot of health benefits. Chili peppers decrease appetite, improve insulin response, reduce oxidation of LDL (which leads to inflammation and a buildup of plaque in arteries), reduce blood clots, and improve endothelial function (blood flow). Seasoning food with peppers decreases the amount of salt needed, which reduces hypertension.
The Moli-Sani study followed 22,811 people over 8 years and found that people who had chili peppers 4 or more times a week had 23% decrease in all cause deaths, 33% decrease in cardiovascular deaths, 44% decrease in ischemic heart disease, and 61% decrease in strokes (NCBI).
When buying chili peppers, fresh ones are best, followed by dried, then followed by hot sauces.
Fresh is best
The closer your food is to how it comes out of the soil or off the tree, the better it is for you. Food produced locally will have more nutrients and less preservatives than food that has been shipped in from out of state or out of the country.
Eat Lots of Fruits and Veggies
During COVID, we saw how diet affects the immune system. Those who ate a plant-based diet had a 72% decrease in developing severe covid and those who ate a pescatarian diet had a 61% decrease in developing severe COVID. Those who eat more fruits and vegetables have stronger immune systems. Seventh day Advantists live an average of 10 years longer than the average American, which is likely attributed to the fact that most eat primarily plant-based diets or are vegetarians or semi vegetarians.
On the other end of the spectrum, those who ate a low carb, high protein diet like the Keto or Atkins diets, had a 50% higher risk in developing COVID and were more likely to have severe COVID symptoms, requiring oxygen, or ICU treatment. While Keto and Atkins diets help you lose weight, they will kill you faster than if you had eaten the standard American diet.
It took us a while to figure out that these diets are unhealthy, because they do lower your cholesterol and blood pressure numbers, but will increase your risk of stroke, heart attack, cardiovascular disease, and increase mortality rate.
Move More
The American Heart Association recommends 150 minutes of exercise a week of moderate exercise or 75 minutes a week of high intensity exercise. Any type of exercise that makes your heart pump, your muscles move, and makes you sweat is great for your health. You can divide this time up however you want throughout the week, but each session should be a minimum of 10 minutes to get the maximum cardiovascular benefit.
How do you know how hard you are exercising? Use the talk test:
- Mild = you can talk and sing while you exercise
- Moderate = you can talk, but you can’t sing (brisk walk)
- High intensity = you cannot talk, you are fighting for air (sprinting)
The more you move throughout the day, the better. Even just going to the grocery store is better for your health than getting your groceries delivered.
Stress Less
Find ways to minimize stress or find ways to better manage your response to stress.
As a medical student, Dean Ornish tested an intensive cardiac rehab program that included a plant based diet, stress management, yoga, exercise, and meditation. Participants were taken to the cardiac catheterization laboratory to look at the blockage in the arteries in their hearts. The study proved that the blockage decreased. If you had a heart attack, bypass surgery, or a stent, you qualify for his program which is covered by Medicare.
Maintain a Healthy Weight
Weight loss should not be your goal, rather it should be a consequence of your healthy lifestyle. By limiting salt and sugar intake, living an active lifestyle, limiting stress, and eating fresh, healthy foods, you will be able to more easily attain and maintain a healthy BMI.
Don’t try things that have not been proven. We have hard data that lifestyle changes make a drastic difference in your longevity and quality of life. Lifestyle medicine is just now starting to be integrated into the curriculum of most medical schools, but it will take time to become mainstream.
Don’t wait to start living a healthier life. Your first symptom of cardiac death will likely be your last. Your health is your most precious asset. Take control.
To learn more, see the full talk below or visit Dr. Teixeira’s website at https://www.doctorstmd.com/.
Dr. Jose Teixeira
MD – Cardiologist, Electrophysiologist
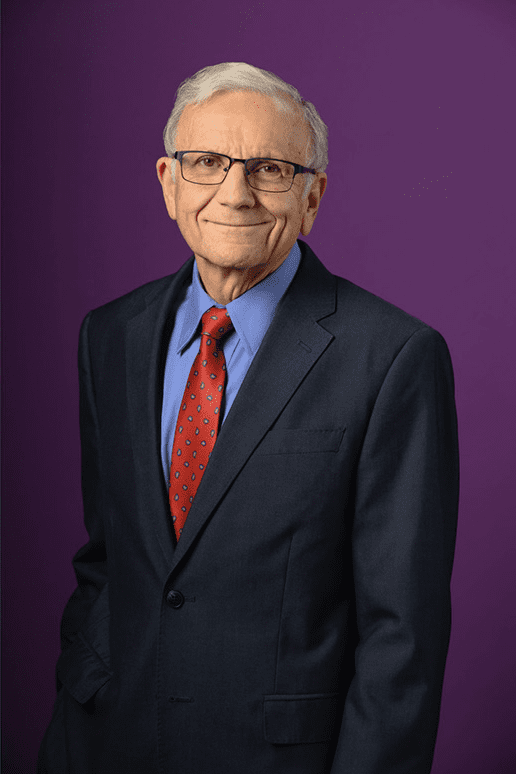
Dr. Jose Teixeira, MD is a well-respected cardiologist and electrophysiologist at Monument Health Heart and Vascular Institute with 46 years of experience. Dr. Teixeira completed medical school at Universidade NOVA de Lisboa in Portugal and a 2 year public health rotation before moving to New York City to undergo Internal Medicine residency training at Interfaith Medical Center. He then completed a fellowship in cardiology and electrophysiology with the University of Medicine and Dentistry of New Jersey (UMDNJ) at Deborah Heart and Lung Center. Subsequently, he joined the University of South Dakota School of Medicine as Chief of Cardiology. In 2019, he became board certified in lifestyle medicine after discovering its ability to prevent, help treat, and reverse disease. He works to help his patients with chronic diseases proactively, ensuring a healthier future.